World Prematurity Day: Honouring the Oliver Fisher Unit
It’s November 17, World Prematurity Day!
22 years ago, my mum was 28 weeks and 5 days pregnant with twins when she suddenly started having contractions. Rushed to the hospital, doctors gave her steroid injections to help their tiny lungs develop. After a night spent in the hospital, my mum was told that she would have to deliver. The room was packed – eighteen people in total: six caring for my mum, and six for each of the twins.
On the 17th November 2003 at 4:44pm, I was born, weighing just 2lbs 7oz.
One minute later, my twin sister arrived at 2lbs 12oz.
I was older, she was heavier, and I’ve never let her forget it.
We spent seven weeks in the Oliver Fisher Unit at Medway Maritime Hospital before we finally went home on January 2nd 2004, each of us weighing around 5lbs.
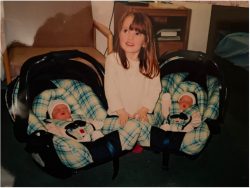
Image: Hannah Colechin / The Boar – 2nd January 2004, the day we were cleared to go home
When I asked my mum what she loved most about the Oliver Fisher Unit, she said that it was how “hands-on” they let her be – teaching her how to change nappies, feed us through tubes, and even pick out tiny, knitted clothing. The environment, she said, was calm, kind, and respectful. But she also said something that stuck with me – that even though it felt peaceful, “not all babies made it.”
Twenty-two years later, I find myself celebrating our birthday and World Prematurity Day (funny coincidence, I know). The day highlights the challenges faced by premature babies like us and the vital importance of quality neonatal care.
I’ve always wanted to show my gratitude to the Oliver Fisher Unit, the place that cared for me and my family over two decades ago. In April 2025, my sister ran the Brighton Marathon, raising over £500 for the Oliver Fisher Special Care Baby Trust. I wanted to contribute too … but in a way that didn’t involve running 26 miles.

Image: Hannah Colechin / The Boar – My sister, raising money for the Oliver Fisher Special Care Baby Trust at the 2025 Brighton Marathon
Instead, I reached out to the Oliver Fisher Special Care Baby Trust and had the incredible honour of interviewing Dr Aung Soe, the charity’s chairman and consultant neonatologist. Soe has dedicated nearly three decades to caring for his patients and their families. Originally from Burma, he came to the UK in 1988, passed the GMC exam, and began working in 1989. Soe completed his neonatology training across Liverpool, Oxford, and London before joining Medway in 1996. By October 2026, Soe will mark 30 years in the field.
When discussing neonatology, Dr Soe described it as a uniquely challenging and rewarding speciality. “Newborns are fascinating because they can’t tell you what’s wrong,” Soe explains, highlighting the intellectual demands of the role. Equally important, Dr Soe enjoys supporting the whole family through what can be a stressful and emotional journey.
He has witnessed enormous changes in both technology and staffing over the years and emphasises his role in guiding parents through difficult outcomes. Encouragingly, Soe notes that even at 23 weeks, there is still potential for normal development, underscoring the possibilities inherent in neonatal care.
Having spent decades caring for pre-term babies, Dr Soe has extensive experience in the particular challenges they face. “The lungs can progress into what we call chronic lung disease, or BPD, Bronchopulmonary Dysplasia,” Soe explains, “a lung condition that almost exclusively happens to pre-term babies. It’s very rare in full-term babies. And that means that the baby will still need oxygen at 36 weeks.”
Pre-term babies are also at risk of brain complications. “They are at risk of what we call intraventricular haemorrhage or IVH, which is very rare in full-term babies because the blood vessel development in the brain is incomplete until you are around 34-36 weeks,” Dr Soe notes. Monitoring for IVH involves careful care: “You would have to bring artificial nutrition through your soft spot regularly until you reach 34-36 weeks.”
Eye and digestive health are also major concerns. “The eye, that is the condition for ROP, retinopathy of prematurity. So that, again, we monitor because it is a leading cause of visual problems in newborn babies in developed countries,” Dr Soe explains. Pre-term infants are also vulnerable to NEC, necrotising enterocolitis, which can cause inflammation or infection in the bowels.
Dr Soe emphasises that the challenges extend beyond immediate medical complications. “With or without IVH, pre-term babies’ brains need to catch up. So neurodevelopmentally, there’s a higher risk of cerebral palsy. There’s a higher risk of developmental delay. So, a baby born under 30 weeks will have detailed developmental assessments when they reach the age of two.”
Clearly, caring for pre-term babies requires a highly specialised environment. I asked Dr Soe to describe the Oliver Fisher Unit itself and how it supports these vulnerable infants. “So, the Oliver Fisher Unit is what we call commission. We have eight intensive care cots. So that is for intensive care support. And also, we look after six high-dependency babies, and then 16 special care cots, and then eight transitional cots,” he explains. “Babies who need breathing support and blood pressure monitoring are categorised as intensive care babies, and then when they get better, they move into high dependency.”
The staffing structure reflects the level of care required. “From a staffing point of view, we have nine consultants and then over twenty resident doctors. And over 100 nurses look after the babies on the unit, with about 12-15 on the unit at one time,” Dr Soe says.
Soe highlights the growing role of allied health professionals. I mention to him that my sister is currently studying Speech and Language Therapy: “Until a couple of years ago, allied professionals, including speech and language therapists and physiotherapists, weren’t available on the unit. Now it’s a national drive. We have speech and language therapists, physiotherapists, and pharmacists. They’re equally important as nurses and doctors.”
Beyond his clinical work, Dr Soe also plays a pivotal role in supporting the Oliver Fisher Unit through the Oliver Fisher Charity, where he serves as Chairman. “So, my predecessor, Dr Tucker, started as a consultant in 1982,” he explains, “and then he opened the intensive care unit in All Saints Hospital (Chatham) in 1984 and then he set up this charity in 1985. So, this year is the 40th anniversary celebration.”

Image: oliverfisherscbt / Instagram – Celebrating 40 years
The charity was designed to provide additional support where NHS resources are limited or highly competitive. “In this hospital, we want breathing machines, ventilators, ultrasound machines … The charity can support what is needed, not only for clinical care but also support for parents.” Dr Soe took over leadership of the charity in 2016 when Dr Tucker retired and describes it as a “privilege” to continue this work.
Over the years, the charity has funded major upgrades to the unit, including a high dependency upgrade costing over £100,000 and a transition care upgrade of more than £300,000. Currently, it is running the IC-e Cream Campaign to improve intensive care, with a commitment of at least £250,000. “We started that in April, and now at the end of October, we’re already halfway,” Dr Soe notes. According to him, the overarching goal of the charity is clear: to ensure the unit has the equipment and resources it needs to provide the best possible care.
Advanced equipment funded by the charity has made a tangible difference in day-to-day care for the patients. “So, when the baby is on a breathing machine, we want to make sure that their oxygen levels are normal,” he explains. Rather than relying solely on blood tests, a small probe placed on the baby’s skin allows the machine to monitor oxygen levels non-invasively. Thanks to the charity, eight of these machines were recently donated, and plans are underway to purchase additional ventilators.

Image: Hannah Colechin / The Boar – an example of the type of equipment used on premature babies
The charity has also supported families directly, donating breast pumps for use on the unit. Dr Soe emphasises the flexibility this provides, explaining how the pumps can be taken home, borrowed when needed, and returned afterwards, helping to maintain feeding routines for pre-term babies.
To round off the interview, I ask Dr Soe what he is most proud of. His answer reflects not just his professional achievements but the profound impact he has had on the lives of the babies and families he cares for. Pointing to photos in his office, he fondly recalls extremely pre-term babies who return years later to say hello, describing these moments as “really rewarding.” Soe mentions the teamwork involved in complex cases, such as quadruplets who required four teams of doctors and nurses, and the fascination of witnessing genetics at work when he delivered a set of triplets.
Dr Soe additionally shares some particularly personal stories: a baby born, at just 28 weeks weighing 405g, invited him to their 18th birthday, and another, born at 27 weeks, is now a qualified paramedic. “I will happily retire in one or two years with all of these memories,” Dr Soe concludes.
It was an honour speaking with Dr Soe, not just as a journalist, but as someone whose life began in the very unit he leads. Following our conversation, I immediately called my mum and my sister to tell them everything. Having been born there 22 years ago, it felt surreal to sit down with the man who has dedicated nearly three decades to the place that gave me my start. World Prematurity Day is all about raising awareness, but for me, it’s also about giving thanks to the doctors, nurses, and families of the Oliver Fisher Unit, who continue to fight for tiny lives every single day.
On this day of World Prematurity, take a moment to celebrate the strength of premature babies, their families, and the incredible people who care for them. With support from the Oliver Fisher Special Care Baby Trust and other charities who support neonatal care, that work can continue for years to come.
To learn more or donate, visit the Oliver Fisher Trust website.
Because in the world of neonatal care, every little counts … and little ones count most of all.

Comments (3)
Such a heartfelt and interesting article! You really shine a light on all the amazing hard work that goes on behind the scenes in neonatal care 🙂
What a fantastic article!
What an enthralling and powerful article from Hannah. My late wife and I have much to be thankful for the work that the Oliver Fisher do. We are the proud Grand Parents of Hannah and Louise Colechin.