SMASH or pass: The new ‘Netflix Style’ model for antibiotic prescription.
In 1929 chemist Alexander Fleming was working at St Mary’s hospital in London where he was unsuccessfully studying how to inoculate against the rampant influenza virus. To combat the severe ‘scientist’s block’ inhibiting his scientific progression, Dr Fleming left his lab for a short holiday to Suffolk in the hope of taking his mind off the failing lab work. In his scurrying exit, Dr Fleming carelessly forgot to sterilise or dispose of a plate containing Staphylococcus bacterium, returning embarrassed to find that mould had colonized the neglected bacterial population. However, upon close inspection, he noticed that presence of small mould spores arrested nearby bacterial growth, and through additional complex chemistry experiments, found this to be achieved through the mould’s production of a ‘self-defence’ substance now referred to as penicillin. Through the tireless effort of other scientists, like Florey, Chain and the ‘Penicillin Girls’ based in Oxford, this substance was transformed into the first druggable antibiotic and strands of penicillin, like amoxicillin, are still the most prescribed antibiotic used today. Despite this initial serendipitous leap, sound drug development not only includes a pre-clinical synthesis of antibiotics but also strenuous clinical tests and marketing strategies making the modern development of antibiotics multi-fold more tricky, expensive and time-consuming than penicillin’s pioneering voyage.
no matter how effective a drug may be, antibiotics must only be used if absolutely necessary
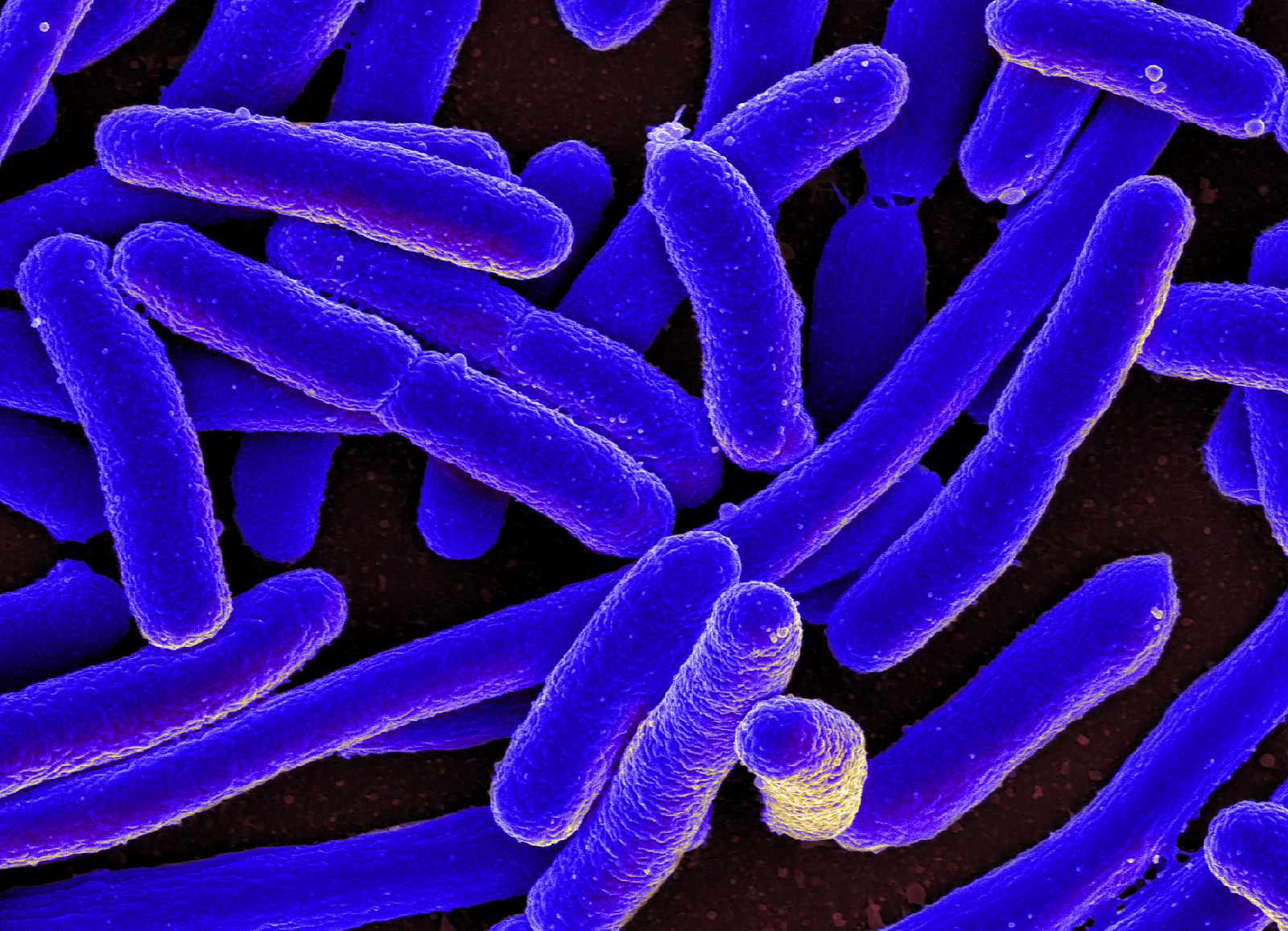
Although a powerful tool in fighting illness, doctors are now strongly advised to reduce their prescription of antibiotics due to the increasing incidence of antibiotic resistance. Antibiotic resistance results from the increased use of antibiotics, meaning pathogens can evolve methods of protection, primarily driven through mutation, to become resistant to the most commonly prescribed drugs. Therefore, no matter how effective a drug may be, antibiotics must only be used if absolutely necessary to minimalize the chances a pathogen develops resistance. The rising incidence of relaxed prescription, which subsequently leads to rising levels of antibiotic resistance, further results in a reduction of novel antibiotic development due to both bacteria becoming more and more difficult to effectively kill with known methods and little economic return with many modern and novel drugs rapidly becoming ineffective against its target bacteria.
With antibiotic resistance on the rise, but no new antibiotics to fall back on, we are left with a major issue. How do we promote antibiotic discovery where there is no economic payoff? Subscription Models for Antibiotics in Hospitals, aka SMASH, were created to address this issue by making research income more stable. Under this scheme, hospitals and trusts will subscribe to the antibiotic and pay a pre-determined rate, irrespective of the drug’s usage. This will allow pharmaceutical companies to make a profit to fund production but still allow hospitals to prescribe fewer drugs. First trialled on July 1st, 2022, by NHS England and the National Institute for Health and Care Excellence (NICE), this novel idea was used for two antibiotics avibactam and cefiderocol.
However, despite being implemented over a year ago the subscription model doesn’t seem to have made much of a difference. A recent survey was done throughout NHS hospitals in England, asking infectious disease or medical microbiology consultants how they thought the SMASH model was working. Only 57% of consultants had even heard of SMASH, which shows that we still have a large way to go in advertising, let alone in evaluating how well the model works. The consensus seems to be a positive outlook towards using SMASH in the future, but with a limited time, it is still yet to be shown whether this will prove effective in the long term with many holding out hope that England will become antibiotic development trendsetters for the rest of the world.
These approaches all provide support for the development of new antibiotics in spite of harsh clinical and economic realities
Though novel with few concrete results, a cacophony of other countries have followed the UK’s venture into drug subscriptions. The USA have proposed the most significant change through the ‘PASTUER Act’. This also involves a subscription, but guarantees antibiotics a 5-year revenue, in contrast to the yearly subscription in the UK. Sweden has further set a minimum revenue guarantee for pharmaceutical companies and both France and Germany have put measures in place that allow companies to get reimbursed if they don’t make a certain amount. These approaches all provide support for the development of new antibiotics in spite of harsh clinical and economic realities. Therefore, although the theory remains solid, only time will tell if it will help in the fight against antibiotic resistance.
The full results can be read here (https://academic.oup.com/jacamr/article/5/Supplement_1/dlac133.027/6991377),
Comments