Research opens doors to first blood test for osteoarthritis
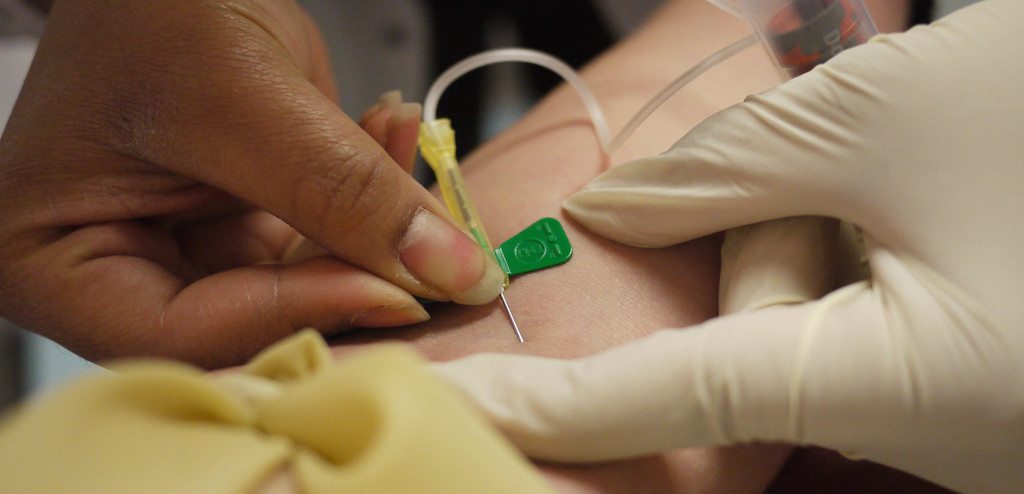
The first blood test for osteoarthritis could soon be developed, due to recent findings from research conducted by Warwick Medical School.
The research identified a biomarker linked to both rheumatoid and osteoarthritis.
Osteoarthritis causes the joints to become painful and stiff as cartilage inside the joints wears away with time. It is the most common type of arthritis in the UK and develops, in most cases, with age.
Rheumatoid arthritis, which occurs more often at a younger age, is caused by immune system cells targeting the joint’s lining.
Tests for rheumatoid arthritis (RA) have already been established, but the newly identified biomarker could lead to the development of a new test that could diagnose both RA and osteoarthritis (OA).
The research focused on citrullinated proteins, a biomarker suspected to exist in the blood of people with early stage RA. The research found increased levels of CPs in both early-stage OA and RA patients.
Using this, they found that a single test could possibly detect and discriminate between the main types of arthritis at the early stages, before any joint damage has occurred.
Lead researcher, Dr. Naila Rabbani said: “This is a remarkable and unexpected finding. It could help bring early-stage and appropriate treatment for arthritis which gives the best chance of effective treatment”.
Dr. Rabbani went on to explain that it had been long established that the autoimmunity of early-stage RA leads to the role of CPs in relation to antibodies too, but the autoimmunity, and therefore the antibodies, are absent in early stage OA.
The research also enabled the team to discriminate between early-stage RA and other inflammatory joint diseases, allowing for earlier diagnosis.
Dr Rabbani said: “This discovery raises the potential of a blood test that can help diagnose both RA and OA several years before the onset of physical symptoms”.
Comments